Erin1
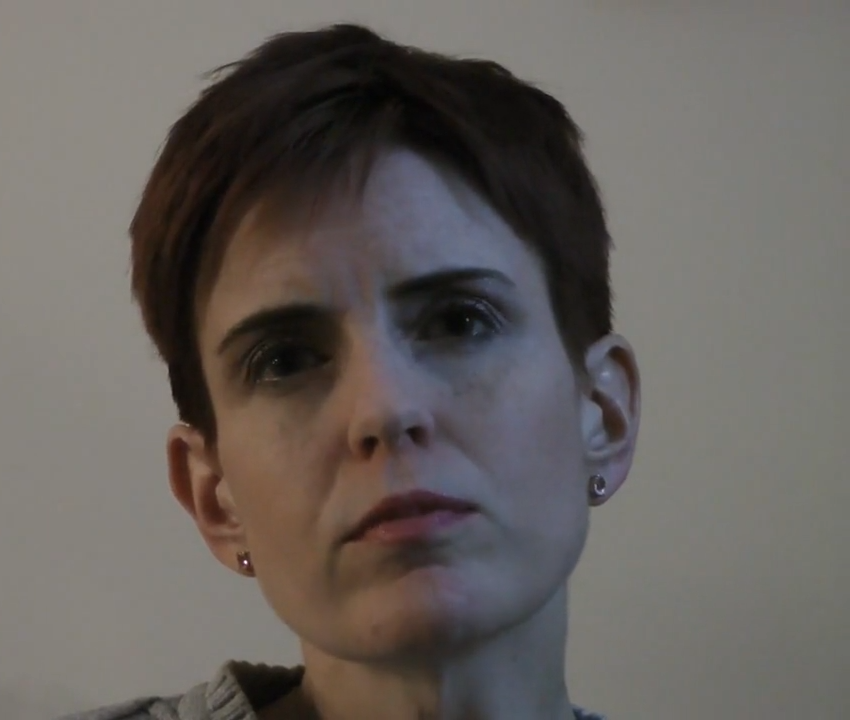
Age at interview: 38
Erin is a 38-year-old woman who lives with her partner and daughter who was one year old at the time of interview. Her son, who was born eight years earlier, lives part-time with Erin and part-time with his father.
Erin has lived with mental health challenges since she was a teenager. Treatment for anorexia and depression included medication, cognitive behavioural therapy and periods of hospitalization. When Erin was planning her first pregnancy, she felt stable and took steps to manage concerns about the changes her body would undergo during pregnancy. For example, she got rid of clothes that would no longer fit, and she was weighed facing away from the scale at medical appointments. She also tried to stay focused on the “end game” of having the baby.
Erin’s first pregnancy went relatively smoothly. She gained weight normally and was able to manage any anxiety and depression. However, at 33 weeks she went into premature labour and was subsequently diagnosed with preeclampsia and a rare, life-threatening complication known as HELLP Syndrome (Hemolysis, Elevated Liver enzymes and Low Platelets – a variant of preeclampsia). Her son’s delivery and the aftermath were traumatic and required life-saving medical intervention for Erin. Her son went to the neo-natal intensive care unit (NICU) and she felt she had to ask permission to have contact with him.
Post-partum, Erin experienced severe anxiety and depression and was unable to eat or sleep normally. She tried repeatedly to convey to family members and healthcare professionals how unwell she felt but no one seemed to be listening. Erin was also seeing a perinatal psychiatrist, but these appointments were very brief and entirely focused on prescribing or adjusting medication that did not seem to be working. Because of the medication, Erin decided not to breastfeed her son, but was confronted with judgmental attitudes from other new mothers and felt uncomfortable attending mother and baby groups.
At four months, Erin put her son into daycare, and this provided some of the respite to manage her own health needs while caring for her baby. She also independently discovered a post-partum mood disorder support group which she began to attend. While it was initially daunting to walk into a room full of strangers, Erin discovered that she was not the only new mother struggling with a mood disorder and she found it extremely helpful to be in the company of other women who did not judge or consider her to be crazy.
Two years after having her son, Erin was hospitalized for severe depression. Given that she had never responded well to any of the many medications she had taken, a psychiatrist reviewed her entire history and revised her diagnosis to Bipolar Disorder Type II. The mood stabilizers she was subsequently prescribed have been much more effective than previous medications.
Eight years after the birth of her son, and feeling stable, Erin decided to try for a second child. As with her first delivery, Erin went into labour prematurely and had to have a Caesarian section. After a couple of weeks, and with her baby in the NICU, she began to experience severe depression. Drawing on her previous experience, Erin went back to the support group she had attended after the birth of her son. With her partner at home as the primary care provider, she was also able to go back to work which she found to be stabilizing.
Erin is now doing well, and her children are happy and healthy. She emphasized the need for more prenatal education and better and more widely available social support for women experiencing post-partum mood disorder.
More content
- Sharing Experiences – Erin1Erin1 found a support group at a community hospital, and it saved her by helping her realize that she's not alone.
- Coping with Perinatal Mental Health – Erin1Erin1 used CBT skills to cope.
- Medication and Treatment Approaches – Erin1Erin1 was treated unsuccessfully for depression before getting the right diagnosis and medication.
- Work, Finances and Mental Health – Erin1Erin1 returned to work while her partner stayed at home, hoping that things would get better.
- Managing Personal Challenges with Sleeping and Eating – Erin1Having had experience with an eating disorder, Erin1 took precautionary steps, knowing her body would change during pregnancy.
- Stigma and Feeling Judged – Erin1 (clip 2)No-one wants to talk about the dark side of having babies but at the same time, Erin1 felt bad for opening up about these topics.
- Stigma and Feeling Judged – Erin1For Erin1, there is a preconceived idea that women with postpartum depression harm their babies.
- Managing New Routines – Erin1Fearing judgement from other mothers while bottle feeding her baby contributed to Erin1's isolation.
- Coping with Feeding – Erin1Erin1 chose to bottle feed due to her medications, but judgements from what she calls 'sancti-mommies' created barriers for her to connect with other mothers.
- First Symptoms – Erin1A few weeks after the birth of her second child, Erin1 began experiencing symptoms that were different from those she had with her first.