John
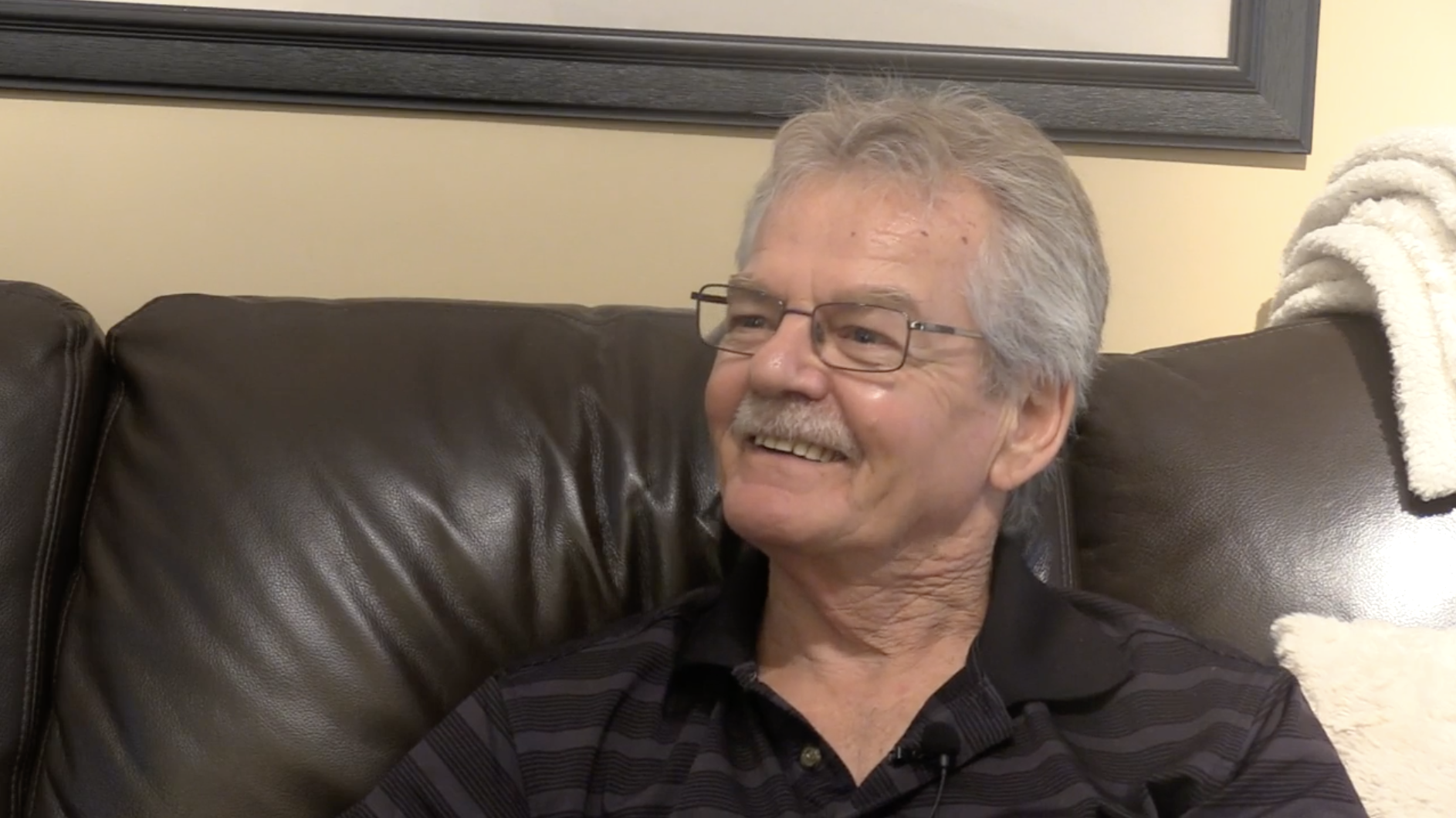
Patient Partner
John is a trained educator, and since retirement from teaching he works part-time as a public educator and patient advocate with a national heart health foundation. John got involved in this work while he was recovering from heart disease. He wanted to learn about how patients can use their voice to have an impact on the care they receive. He also wanted to learn about how men and women each experience heart disease, particularly as he had unusual symptoms himself. His own health experience led him to get involved in a research project about heart health at a local university. He helped to search for articles related to the project, prepare grant submissions, and develop educational resources for patients. John had formal research partnership training through an online course that he found informative. He feels that patients/caregivers should be provided with training to help increase their confidence and ability to contribute to the research process. He also suggests that researchers create defined roles for patients/caregivers and be clear about what is expected of all involved to ensure that the engagement in research partnerships has real value. John looks forward to continuing his involvement in research and feels that others who are interested should get involved because patient experience is so important in shaping research priorities around patient care.
More content
- Improving Patient Care and Experiences – JohnEngaging in research activities has influenced John’s approach to his own healthcare management
- Improving Patient Care and Experiences – JohnJohn has observed that engaging patients as partners in research is new for some researchers and may involve a learning curve
- Advice to others – JohnPatients’ and caregivers’ stories can make a difference to doctors, physicians and researchers - John encourages the sharing of experiences
- Path to involvement – JohnWhile recovering from heart disease, John joined heart health initiatives that led to an opportunity